Universal Definition of Myocardial Infarction
Contents [hide]
- 1 Criteria for type 1 MI
- 2 Criteria for type 2 MI
- 3 Criteria for type 3 MI
- 4 Type 4a MI -Criteria for PCI-related MI 48 h after the index procedure
- 5 Type 4b myocardial infarction- Stent/scaffold thrombosis associated MI
- 6 Type 4c myocardial infarction -Restenosis associated MI
- 7 Type 5 MI – CABG-related MI
- 8 Criteria for CABG-related MI 48 h after the index procedure (type 5 MI) CABG-related MI is arbitrarily defined as elevation of cTn values
Criteria for type 1 MI
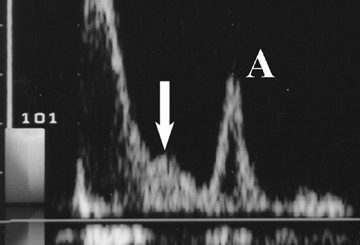
Detection of a rise and/or fall of cTn values with at least one
value above the 99th percentile URL and with at least one of the
following:
• Symptoms of acute myocardial ischaemia;
• New ischaemic ECG changes;
• Development of pathological Q waves;
• Imaging evidence of new loss of viable myocardium or new
regional wall motion abnormality in a pattern consistent with
an ischaemic aetiology;
• Identification of a coronary thrombus by angiography including intracoronary imaging or by autopsy
Criteria for type 2 MI
Detection of a rise and/or fall of cTn values with at least one value
above the 99th percentile URL, and evidence of an imbalance
between myocardial oxygen supply and demand unrelated to acute
coronary athero-thrombosis, requiring at least one of the following:
• Symptoms of acute myocardial ischaemia;
• New ischaemic ECG changes;
• Development of pathological Q waves;
• Imaging evidence of new loss of viable myocardium or new
regional wall motion abnormality in a pattern consistent with
an ischaemic aetiology.
Criteria for type 3 MI
Patients who suffer cardiac death, with symptoms suggestive of
myocardial ischaemia accompanied by presumed new ischaemic
ECG changes or ventricular fibrillation, but die before blood samples for biomarkers can be obtained, or before increases in cardiac biomarkers can be identified, or MI is detected by autopsy
examination.
Coronary intervention-related MI is arbitrarily defined by an elevation of cTn values more than five times the 99th percentile URL in patients with normal baseline values. In patients with elevated pre-procedure cTn in whom the cTn level are stable (<_ 20% variation) or falling, the post-procedure cTn must rise by 20%. However, the absolute post-procedural value must still be at least five times the 99th percentile URL.
In addition, one of the following elements is required:
• New ischaemic ECG changes;
• Development of new pathological Q waves;
• Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality in a pattern consistent with an ischaemic aetiology;
• Angiographic findings consistent with a procedural flow-limiting complication such as coronary dissection, occlusion of a major epicardial artery or a side branch occlusion/thrombus, disruption of collateral flow, or distal embolization.
Type 4b myocardial infarction- Stent/scaffold thrombosis associated MI
Stent/scaffold thrombosis associated with percutaneous coronary intervention (type 4b myocardial infarction)
Type 4c myocardial infarction -Restenosis associated MI
Restenosis associated with percutaneous coronary intervention (type 4c myocardial infarction)
10 times the 99th percentile URL in patients with normal baseline cTn values. In patients with elevated pre-procedure cTn in whom cTn levels are stable (<_ 20% variation) or falling, the postprocedure cTn must rise by > 20%. However, the absolute postprocedural value still must be > 10 times the 99th percentile
URL.
In addition, one of the following elements is required:
• Development of new pathological Q waves;
• Angiographic documented new graft occlusion or new native
coronary artery occlusion;
• Imaging evidence of new loss of viable myocardium or new
regional wall motion abnormality in a pattern consistent with
an ischaemic aetiology