Hypertensive Heart Disease
A. 120 / 80
B. 130 / 90
C. 130 / 80
D. 140 / 80
ANSWER
A. 120 / 80
————–
Current 2017 American Cardiology Association/American Heart Association guidelines define hypertension as blood pressure as systolic blood pressure higher than 120 mm Hg or a diastolic pressure more than 80mm Hg
A. 140 / 90
B. 130 / 80
C. 120 / 70
D. 115 / 75
ANSWER
D. 115 / 75
————–
The risk of cardiovascular mortality doubles for every 20mmHg systolic and 10mmHg diastolic pressure increase over a baseline blood pressure of 115/75.
A. Increase in ventricular wall compliance
B. Reduction in ventricular wall compliance
C. Increase in atrial wall compliance
D. Reduction in atrial wall compliance
ANSWER
B. Reduction in ventricular wall compliance
————–
Abnormal S4 sound on auscultation indicates stiff, hypertrophic ventricles and is very specific to hypertensive heart disease.
A. Systolic heart failure
B. Ventricular septal rupture
C. Atrial fibrillation
D. Reduction in atrial filling time
ANSWER
A. Systolic heart failure
————–
abnormal S3 indicates thin, eccentric hypertrophy associated with systolic heart failure.
A. Low-pitched sound
B. Occurs shortly before the first heart sound
C. Increase intensity in Atrial fibrillation
D. Coincident with late diastolic filling of the ventricle
ANSWER
C. Increased in Atrial fibrillation
It is absent in AF
————–
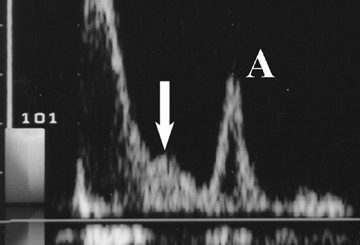
Fourth heart sound
– Low-pitched sound
– Coincident with late diastolic filling of the ventricle
– Produced due to due to atrial contraction.
– Occurs shortly before the first heart sound.
Although it is also called the atrial sound, and its production requires an effective atrial contraction, the fourth heart sound is the result of vibrations generated within the ventricle.
S4 – Almost always abnormal
A. 2,000
B. 2,300
C. 2,500
D. 2,800
ANSWER
B. 2,300
————–
American Heart Association recommends no more than 2,300 milligrams (mg) a day and moving toward an ideal limit of no more than 1,500 mg per day for most adults.
High Sodium Diet – greater than 3g/day
A. 110
B. 120
C. 130
D. 135
ANSWER
B. 120
————–
The 2015 SPRINT trial demonstrated a reduced risk of progression to heart failure in patients with more intensive blood pressure control with a target systolic blood pressure of 120mmHg (1.3%) compared with 140mmHg (2.1%).
A. withdrawal of vasodilator effects of endogenous estrogen
B. increased arterial stiffness
C. increased salt sensitivity
D. decreased angiotensin II receptor expression
ANSWER
D. decreased angiotensin II receptor expression
There is increased angiotensin II receptor expression in Postmenopausal State.
————–
After menopause, there is an increase in SBP which is thought to be secondary to the withdrawal of vasodilator effects of endogenous estrogen, increased arterial stiffness and salt sensitivity, diminished endothelial nitric oxide production, and increased angiotensin II receptor expression
In-Shorts
Normally, BP varies with the circadian clock: it is higher during the day time, and decreases by 10% to 20% during sleep, a phenomenon known as dipping.
Patients with a diminished nocturnal BP fall or a nocturnal BP rise, termed nondippers, have a greater prevalence of coronary events, strokes, cardiovascular mortality, and total mortality.
Reverse-dippers – a specific subtype of nondippers in whom BP rises at night.
Reverse-dippers – are at increased risk of CVD.
White-coat hypertension is defined as elevated in-office BP (≥140/90 mm Hg) and normal ABP (awake day-time ABPM <135/85 mm Hg) in individuals not receiving antihypertensive therapy.
White-coat hypertension is generally considered a benign hypertension phenotype
Masked hypertension is defined as normal in-office BP and elevated ABPM (awake day-time ABPM >140/90 mm Hg).
Risk factors include male sex, older age, in-office prehypertension, and diabetes mellitus.
Masked hypertension is a well-known CVD risk factor,